SCHAGHTICOKE — In the past year and a half, Mary Beth Delarm’s visits to her elderly mother have grown increasingly distressing.
Her then 90-year-old mother was a resident of Diamond Hill Nursing and Rehabilitation Center in Schaghticoke, a facility whose persistently poor record of resident care made it a candidate last year for inclusion on a federal watch list.
Whenever Delarm would show up, she said, she’d find her mother in a state of neglect — her body and clothes dirty and unwashed, a soiled diaper unchanged. Sometimes there would be feces smeared around the room, Delarm said. Sometimes her mother had unexplained bruises.
Then there were the gradual yet alarming changes in her mother's condition — a 50-pound weight loss in under a year, and teeth falling out from what Delarm suspected was lack of regular dental care.
She began to document her visits with photos and notes: “Constantly found wet. Yet staff said they were too busy to change her. This was a regular response,” she wrote about one photo.

Mary Beth Delarm began documenting visits to her mother at the Diamond Hill nursing home in Schaghticoke last year. She believes her mother, who is in her 90s and has dementia, was being neglected based on the conditions she often found her in.
ProvidedThat was staff’s response to most complaints, Delarm alleges. She brought her concerns to administration and eventually began reporting them to the state. But in her view, nothing changed. And without guardianship rights, she couldn’t move her mother to another facility.
Now that coronavirus has made its way into Diamond Hill and prevented Delarm from visiting, she’s even more concerned. In fact, she doesn’t even know if her mother is dead or alive. She doesn’t have a direct line to her mother’s room, and no one from the facility has called her back.
Diamond Hill CEO Ari Grinspan did not respond to a request for comment. Clara Tryon, administrator at the home, said she wasn't able to comment and hung up before the Times Union could ask any more questions.
“These places have to be held accountable,” Delarm said. “I don’t want to hear, ‘Oh, we’re so short-staffed’ or ‘We’re so busy.’ It’s a profiteering game to them.”
While much attention has been paid in recent weeks to a state directive that may have helped fuel the coronavirus crisis in New York’s nursing homes, advocates contend that longstanding issues at these facilities similar to those alleged by Delarm played a role as well.
“Obviously nursing home residents are a demographic that is particularly vulnerable to COVID-19,” said Richard Mollot, executive director of the Long Term Care Community Coalition, a nonprofit that advocates for safer nursing homes. “But the lack of sufficient staff in nursing homes on a regular basis, the lack of providing basic infection control and prevention, and other failures in care that have persisted in our nursing homes for years undoubtedly exacerbated the situation.”
A Times Union review of 10 nursing homes in the Capital Region with the largest or deadliest known coronavirus outbreaks found many have struggled to maintain adequate staffing and were cited for infection control violations over the years.
All 10 homes had staffing levels below the minimum recommended level for direct care in the months leading up to the crisis, according to a non-profit advocacy group's analysis of payroll data submitted to federal regulators. And seven of the 10 were cited for at least one infection-control violation during annual inspections in the past three years.
Nursing home leaders interviewed for this story disputed any suggestion that short staffing or poor infection control was a factor in the scale of their outbreaks. They said there was little they could do to keep out a virus that spreads among asymptomatic people, and some said the controversial state policy requiring nursing homes to admit COVID-19 patients from hospitals is just one example of how Gov. Andrew M. Cuomo's administration left nursing homes to fend for themselves in the early days of the pandemic.
“Was that the best policy? Hindsight is always 20/20. We can always second-guess a decision that someone has made,” said Bruce Gendron, vice president of the Grand Healthcare System, which has two facilities with large outbreaks in the Capital Region. “There is no villain in this scenario except for the coronavirus.”

A 518 Rainbow Hunt sign is seen in a resident's window at The Grand Rehabilitation and Nursing at Guilderland on Wednesday, May 6, 2020 in Guilderland, N.Y. (Lori Van Buren/Times Union)
Lori Van Buren/Albany Times UnionShort-staffed
While mistakes are inevitable in any industry, evidence shows that staffing shortages — especially chronic ones — make them far more likely.
Staff with too many residents to care for are simply less likely to have time for basic infection control and prevention practices, Mollot said. That includes things as fundamental as hand-washing or sterilizing equipment before administering care.
“If you read any of the (inspection) citations, they don’t explicitly say it’s because (the facilities) are short-staffed,” Mollot said. “But they’ll say things like, ‘Aide said she didn’t have time.’ That, to me, is emblematic of a staffing issue.”
In the months leading up to the pandemic, most New York nursing homes failed to maintain staffing levels that experts have determined are sufficient for meeting residents’ needs, according to an analysis by Mollot’s organization of payroll data submitted to the federal Centers for Medicare and Medicaid Services (CMS).
In the final three months of 2019, New York nursing homes averaged 3.4 direct care hours per resident day (HPRD) and 0.46 registered nurse hours per resident day, according to the analysis. Minimum recommended levels are 4.1 HPRD for direct care staff and 0.75 HPRD for RN staff.
“My biggest concern in February, back when all this was starting, was that the lack of staffing would make residents that much more vulnerable,” Mollot said.
In the Capital Region, nursing homes with the largest or deadliest known outbreaks of coronavirus all fell short on recommended staffing levels.
Diamond Hill, where Delarm’s mother lived, averaged 2.6 HPRD among direct care staff and 0.3 HPRD among RN staff in the final quarter of 2019. The facility has had 80 confirmed cases of coronavirus among residents and staff, and 16 virus-related deaths.
The nine other facilities reviewed by the Times Union also fell short. They include Shaker Place in Colonie, Hudson Park in Albany, Our Lady of Mercy Life Center in Guilderland, Teresian House in Albany, The Grand in Guilderland, Pine Haven in Philmont, The Grand at Barnwell in Valatie, Glens Falls Center in Queensbury, and Fort Hudson Nursing Center in Fort Edward.
Teresian House — where over 120 cases and 17 deaths from the virus have occurred — was the only facility to exceed the recommended direct care staffing levels at 4.2 HPRD. It fell short on recommended RN staffing, though, with 0.5 HPRD.
A spokesman for the facility, Paul Larrabee, said its staffing was adequate at the time of the outbreak.

A view of the Teresian House Center for the Elderly on Tuesday, May 5, 2020, in Albany, N.Y. (Paul Buckowski/Times Union)
Paul Buckowski/Albany Times UnionLarry Slatky, executive director of Albany County-owned Shaker Place, wrote to the Times Union that at the time the facility learned of its very first COVID case, staffing levels met the facility's resident care requirements based on case mix.
"While we understand the commonly used minimum staffing guidelines, it is impossible to compare one nursing home to another since each nursing home has a unique case mix," Slatky wrote.
Other nursing homes affiliated with larger parent organizations, including Our Lady of Mercy Life Center and Glens Falls Center, said they were able to draw on staff from other facilities in their network as their staffing needs increased during the outbreak. But federal health officials who reviewed virus spread in other parts of the country have said this practice may have actually contributed to virus spread among multiple facilities.
Gendron, who spoke on behalf of the Grand’s Guilderland and Barnwell facilities, said staffing is a challenge across the industry, especially upstate.
“Put simply, demand exceeds supply,” he said.
Advocates point out that retention is the real issue. Staff are underpaid and overworked, resulting in high turnover and constant training of new staff.
New York lawmakers have pushed over the years for changes to state legislation that would require nursing homes and hospitals to implement minimum staffing ratios, but none have come to fruition. A state study on the topic is five months overdue.
Infection control
As coronavirus was bearing down on parts of the U.S., CMS announced in March it would conduct focused infection-control surveys at nursing homes to ensure they were prepared for a possible virus outbreak.
An initial wave of surveys during the week of March 30 found that 36 percent of facilities were not following proper hand-washing guidelines and 25 percent failed to demonstrate proper use of personal protective equipment (PPE) — which has been in use at nursing homes for decades.
Facility-specific results from those surveys have yet to be published. But inspection results dating back to 2017 show that seven of the 10 facilities the Times Union reviewed for this story were cited at least once for infection-control violations.
The Grand Rehabilitation and Nursing at Barnwell, a facility in Valatie with over 160 cases of COVID-19 and 14 virus-related deaths, was cited three times — once in 2017 and twice in 2018.

A view of The Grand Rehabilitation and Nursing at Barnwell on Tuesday, May 19, 2020, in Valatie, N.Y. (Paul Buckowski/Times Union)
Paul Buckowski/Albany Times UnionState health inspectors cited the home in October 2018, when flu season was getting underway, for failing to maintain contact precautions on residents who had been placed in isolation. Such precautions require the use of PPE when entering a patient’s room, which must be clearly marked to indicate protections are needed.
A nurse at Barnwell who requested anonymity for fear of retaliation told the Times Union this month that staffing shortages are putting residents in harm’s way.
“I work doubles,” she said. “You have aides that are working overtime. You’ve got one aide for 40 people and then one nurse. We’ve got to feed, pass trays, do meds, do treatments, answer bells. It’s just impossible. It is bound to lead to poor infection control. There is no way around it.”
Grand Healthcare System's Gendron said the virus strained staffing levels at Barnwell as workers fell sick. The company wound up closing two units and transferring those residents to other Grand facilities in an effort to make patient-staff ratios more manageable.
He downplayed prior inspection-control citations by noting that over 60 percent of all nursing home facilities have been cited for such issues in the past three years.
Other area nursing homes downplayed them, too.
Jeffrey Jacomowitz, a spokesman for the Centers Health Care-owned Glens Falls Center, which has lost at least 19 residents to the coronavirus, wrote to the Times Union that the facility’s most recent citation in 2019 was for a “wound care procedural hand-washing deficiency that resulted in no harm.”
“As leadership from Glens Falls Center and corporate take every deficiency seriously, this very minor citation led to a re-education of clinical and non-clinical staff on proper hand washing and disinfecting of various medical equipment and first aid materials,” he said.
A spokesman for Pine Haven nursing home in Philmont, Columbia County, Geoff Thompson, wrote in a response to Times Union questions about the facility’s past infection control citations that in 2017 Pine Haven was cited for an incident involving a housekeeper that “had no bearing on patient care,” Thompson wrote. Also in 2019, Pine Haven received a state citation that related to human resources education for new hires concerning pneumonia vaccine. Thompson wrote it was “unrelated to patient care.”
“When the crisis broke wide open in March, a lot was not known about COVID-19,” Thompson wrote. “We along with other healthcare providers are continuing to analyze the multiple factors that came into play.”
Pine Haven, which saw 14 out of 36 residents die who contracted the disease, took in one COVID-19 positive patient. And while Thompson did not discuss if that action exacerbated Pine Haven’s outbreak, he wrote “those with COVID need to be treated and remain in a hospital setting.”
Advocates for safer nursing homes say states have long done a poor job of citing the extent to which problems occur inside nursing homes, as well as the extent to which they put residents in harm’s way.
A recent Kaiser Health News analysis found that 99 percent of all infection-control violations are cited as “minor and not warranting fines,” even though 1 million to 3 million serious infections occur inside long-term care facilities each year and 388,000 residents die annually as a result.
On their own?
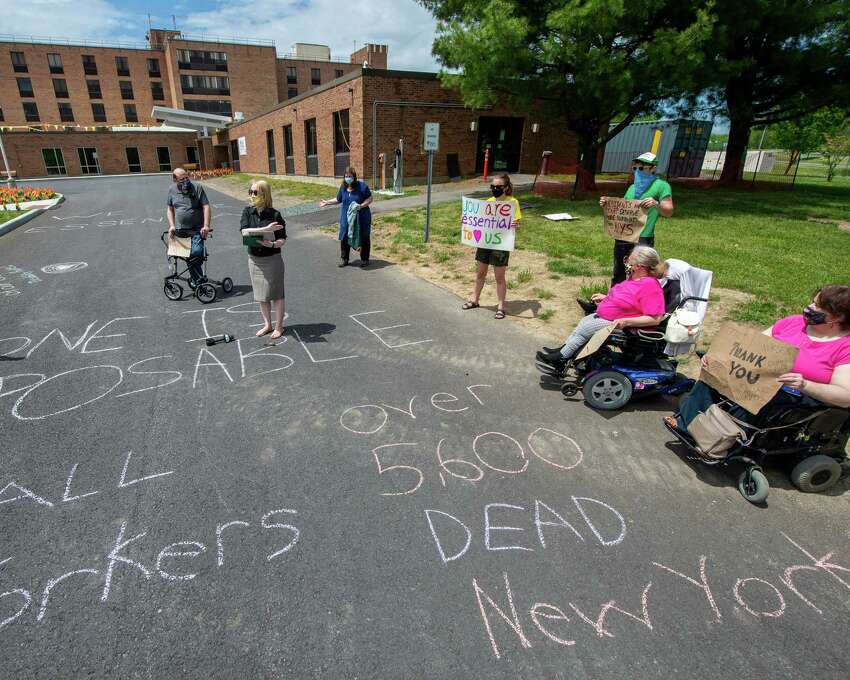
More than 5,800 nursing home residents in New York have died from the coronavirus — a figure that is almost surely an undercount because it doesn't include residents who were transferred to hospitals before they died.
Some area nursing homes with large or particularly deadly coronavirus outbreaks said they did what they could to keep residents safe, but were hampered by factors outside their control and received little support from the state.
Our Lady of Mercy, where 14 out of 44 infected residents died, took in three COVID-19 positive patients. But the facility, which runs underneath the umbrella of St. Peter’s Health Partners, described those patients to the Times Union as in the “recovery phase,” and a spokesman did not have criticisms about any state policies made during the pandemic.
“It started to spread before we even knew we had a single case in our building,” wrote Our Lady spokesman Rob Puglisi. “That was in March, before it was understood that people could test negative and carry the disease for several days with no symptoms, so we had no indications.”
While a state directive requiring nursing homes to accept COVID-19 patients has received a lot of attention (more than 4,500 virus patients were admitted into nursing homes as a result of the directive, an Associated Press investigation found), some area nursing home leaders said they were more concerned that their pleas for help went ignored.
Larrabee, the spokesman for Teresian House, said the facility asked state and local health officials repeatedly for help testing its entire workforce and resident population. “Those requests were rejected,” he said.
The home eventually went out and got the tests itself, he said, and the entire facility was tested April 29. There have been no new cases discovered since then, he said.
Andy Cruikshank, CEO of the Fort Hudson Nursing Center in Fort Edward, which had 40 cases and 11 virus-related deaths, said it felt like the state abandoned nursing homes during the early stages of the pandemic. Cuomo was focused heavily on fighting for more ventilators and hospital beds, while nursing homes including Fort Hudson didn’t even have tests for residents and staff.

CEO Andy Cruikshank stands outside the Fort Hudson Nursing Home on Tuesday, July 22, 2014 in Fort Edward, N.Y. (Lori Van Buren / Times Union)
Lori Van Buren/Albany Times UnionAfter backlash for its handling of nursing homes, the state this month rescinded the controversial admittance policy and announced it would be requiring twice-a-week testing of nursing home staff. But Cruikshank contended that Cuomo's team offered no guidance on how facilities were to pay for such a massive undertaking.
“With employees tested twice a week, the expectation was nursing homes would miraculously coordinate lab contracts (and) they would have to pay for it themselves,” he said. “(Cuomo’s) initial reaction was nursing homes ... are on their own.”
“At no time did the (state) commissioner of health ask, ‘What do you need to make this better?’” Cruikshank added. “The result is a discoordinated approach.”
RELATED: Cuomo defends nursing home policies as long-term care deaths top 5,800
In a statement, the state Department of Health did not respond to the testing concerns raised by the facilities, but noted that it provided both Teresian House and Fort Hudson with thousands of pieces of PPE since the outbreaks, including gowns, face shields, gloves, hand sanitizer, oxygen concentrators and more.
"We've said from the start that protecting our most vulnerable populations including people in nursing homes and adult care facilities is our top priority," department spokeswoman Jill Montag said. "To do so we have issued (Centers for Disease Control)-supported guidance documents, led more than 650 COVID-19 focus infection control surveys and opened 3,000 complaints. We’ve restricted visitors, ordered workers to be temperature checked every day, tested staff twice a week, provided 13 million pieces of PPE and taken other actions to protect this vulnerable population."
Lauren Stanforth contributed reporting for this story.
"short" - Google News
May 31, 2020 at 06:47AM
https://ift.tt/2AkRJma
Was short staffing to blame for Capital Region nursing home outbreaks? - Times Union
"short" - Google News
https://ift.tt/2SLaFAJ































No comments:
Post a Comment